Fact:
-
WHO has declared that AMR is one of the top 10 global public health threats facing humanity.
-
Babies infected with superbugs are dying due to drug resistance in birth facilities within 72 hours of being born.
-
Infections caused multi-drug resistant bacteria kills around 700,000 people each year : WHO
-
Globally, about 35% of common human infections have become resistant to available medicines leading to 700,000 people die every year.
-
By 2040, 12.4% of patients in the country will have multi drug resistance
What is Anti-Microbial Resistance?
Anti-microbial resistance (AMR) is the ability of micro-organisms that cause disease to withstand attack by anti-microbial medicines.
Increasing resistance of pathogens to currently available antibiotics can lead to a situation where advanced techniques and procedures in the field of surgery and medicine become redundant and ineffective due to our failure to prevent the spread of infection
Why does Anti-microbial Resistance occur?
-
Primary reasons:
-
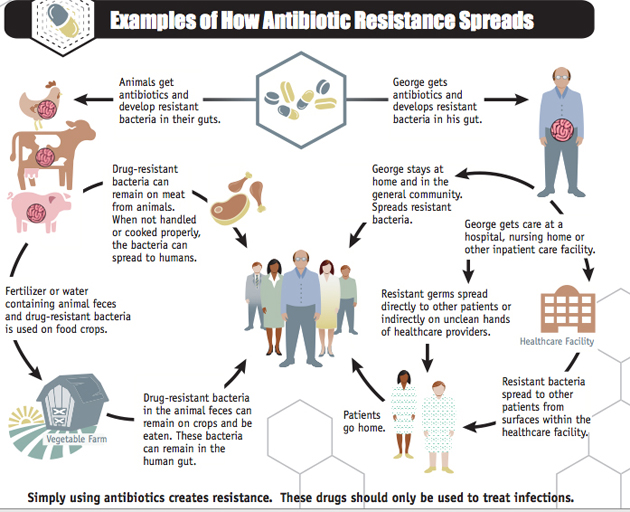
Misuse of antimicrobials in medicine :This happens when the proper course of medication is not done or the person indulges in self-medication.
-
Inappropriate use in agriculture : Antibiotics are used to boost the productivity of livestock.
-
Contamination around pharmaceutical manufacturing sites : The untreated waste releases large amounts of active antimicrobials into the environment.
-
Inadequate wastewater treatment facilities: India has the capacity to treat only about 37% of the sewage generated annually.
-
-
Secondary Reasons:
-
No new antimicrobial developments:
-
No new classes of antibiotics have made it to the market in the last three decades. This is a result of inadequate incentives for their development and production.
-
A recent report from the non-profit PEW Trusts found that over 95% of antibiotics in development today are from small companies.
-
-
Easily Availability: Antimicrobials are easily available as ‘over the counter drugs’ in many countries. This ease facilitates more consumption and development of AMR.
-
Challenges posed by AMR development:
-
Threat to the health care system: Antimicrobials prevent infections post a routine surgery or cancer treatment. Their ineffectiveness would impair the modern health system.
-
Loss of Human Lives: It is responsible for up to 7 lakh deaths a year. It is estimated that 10 million annual deaths would be caused by it post 2050.
-
Economic Brunt: The countries would require abundant capital to manage the AMR crisis in the future. As per an estimate, it may cost up to $100 trillion by 2050.
What is a Super bug?
Microbes that are resistant to multiple antibiotics are called Multi Drug Resistant or Super bug. Ex. NDM-1 superbug.
What is “Chennai Declaration” in this regard?
It is a declaration put together by a small team of professionals against antimicrobial resistance in India. The ‘Chennai Declaration’ created awareness among the medical fraternity about the need to control antibiotic usage
AMR can be counter by:
-
Use: As per the WHO report 2014. People should only use prescribed Antibiotic for full period of prescription. Awareness among people regarding AMR is necessary.
-
Prescription: Health workers and pharmacist must only issue antibiotic when prescribed and prescribing only in required situation.
-
Research and Cooperation: Research on new drugs should be carried out in a speedy manner. International cooperation to fight together and check this menace is prerequisite.Incentivisation: The companies must be encouraged to develop new antimicrobial drugs. In this regard, a multi-sectoral $1 billion AMR Action Fund was launched in 2020 to support the development of new antibiotics.
-
Regulation: Strict and comprehensive legislation for limiting use of antibacterial in livestock which are the cause of transfer of superbugs or resistance microorganisms in humans.
-
Global Coordination: International alignment and coordination are paramount in both policymaking and its implementation. The countries can use the Paris Agreement as a blueprint for developing a similar global approach to tackling AMR.
Measures adopted to fight AMR:
-
Identified as the emerging issue of environmental concern:
-
Highlighted in the United Nations Environment Programme’s (UNEP)’s 2017 Frontiers Report.
-
UN Environment Assembly pressed the need to further understand the role of environmental pollution in spreading AMR.
-
-
One Health AMR Global Action Plan (GAP): by UN agencies to addresses the AMR issue in human, animal, and plant health and food and environment sectors.
-
Draft for setting the residues of 121 antibiotics in treated effluents: from drug production units was issued by Ministry of Environment, Forest and Climate Change (MoEF&CC)
-
Inter-ministerial Steering Committee on AMR: was constituted by the Ministry of Health and Family Welfare and MoEF&CC with representation from the World Health Organisation and UNEP.
Why India is more vulnerable?
-
As per studies AMR is higher in developing countries as compare to developed world.
-
Bacteria spreads easily as about 50% defecate in open.
-
Sewage is not treated.
-
As a result, Indians have among the highest rates of bacterial infections in the world and collectively take more antibiotics, which are sold over the counter here, than any other nationality.
-
Also, all those drugs that create resistance to antibiotics find their way into hospital sewage, which is mostly dumped untreated into rivers, canals and pits in the surrounding community where pregnant women can become infected.
-
Rapidly growing India’s industrialized animal husbandry where antibiotics is widely used.
-
Most large chicken farms here use feed laced with antibiotics banned for use in animals in the United States. A New Delhi science group recently found antibiotic residues in 40% of chicken samples tested.
What India is doing innovative in this regard?
-
India’s has implemented a model of putting a red line on antibiotic packages to curb their over-the-counter sale. This model can be used globally to counter the rising threat of superbugs.
-
Its aim is to curb irrational use of antibiotics and create awareness on the side effects of taking antibiotics without prescription. Under it, all prescription only antibiotics should be marked with a vertical red line on the packets.
Other Steps taken:
-
Government has announced a National Action Plan to combat AMR. The National action plan has objectives of enhancing awareness, strengthening surveillance, improving rational use of antibiotics, reducing infections and promoting research
-
Indian Council of Medical Research (ICMR) has set up a National Anti-Microbial Resistance Research and Surveillance Network (AMRRSN) to enable compilation of data of AMR at the national level.
-
Health ministry enacted regulations to regulate the sale of antibiotics and brought out National Guidelines for the use of antibiotics.
-
National Programme for Containment of AMR is under implementation in 12th Five Year Plan with the following objectives:
-
To establish a laboratory-based surveillance system by strengthening laboratories.
-
To generate quality data on AMR for pathogens of public health importance.
-
To generate awareness among healthcare providers and in the community regarding the rational use of antibiotics.
-
To strengthen infection control guidelines and practices and promote rational use of antibiotics.
-